Pelvic Congestion Syndrome: Treatment, Causes, Symptoms, Diagnosis
Overview:
Pelvic congestion is the
condition in which women experience unexplainable pain in the pelvic area that
lasts more than 6 months. This is due to
the swelling of the veins in their pelvis. Pelvic syndrome is not common in
young women with more than one child.
The symptoms include irregular
pain in the lower back, pelvis, and upper thigh, pain during sex, and
discomfort after sex. The symptoms may worsen as the day progresses and are intensified
by being active or standing for extended periods. The symptoms include pain in
the pelvis, lower back, and upper thigh that does not follow a regular pattern.
Pain during, and after sex are also common1.i
Special X-rays, called
venography, were previously required for pelvic congestion diagnosis. However,
ultrasound alone is often sufficient. Treatment options are medications,
minimally invasive procedures (embolization), and sometimes healthcare
providers recommend surgery. You can treat this condition by lifestyle
changes.
What is Pelvic Congestion Syndrome?
Pelvic congestion syndrome is a rare and not well-understood
condition that can cause ongoing pelvic pain in women before menopause. It's
linked to swollen veins in the pelvic area and the pain can get worse when you
stand for a long time, during sex, periods, or pregnancy.
How common is Pelvic congestion syndrome?
Pelvic congestion syndrome is not very common. It's considered a
rare condition.
How serious is Pelvic congestion syndrome?
Pelvic congestion syndrome can lead to disability if left untreated. Approximately one-third of women experience chronic pelvic pain in their lifetime.
At what age women are at high risk of PCS?
Women who can have children and have been pregnant more than once may be at the highest risk of getting pelvic congestion syndrome.
Symptoms:
What are the symptoms of PCS?
Symptoms of PCS may include any
of the following:
- Low back pain
- Vaginal discharge
- Abnormal vaginal bleeding
- Hemorrhoids
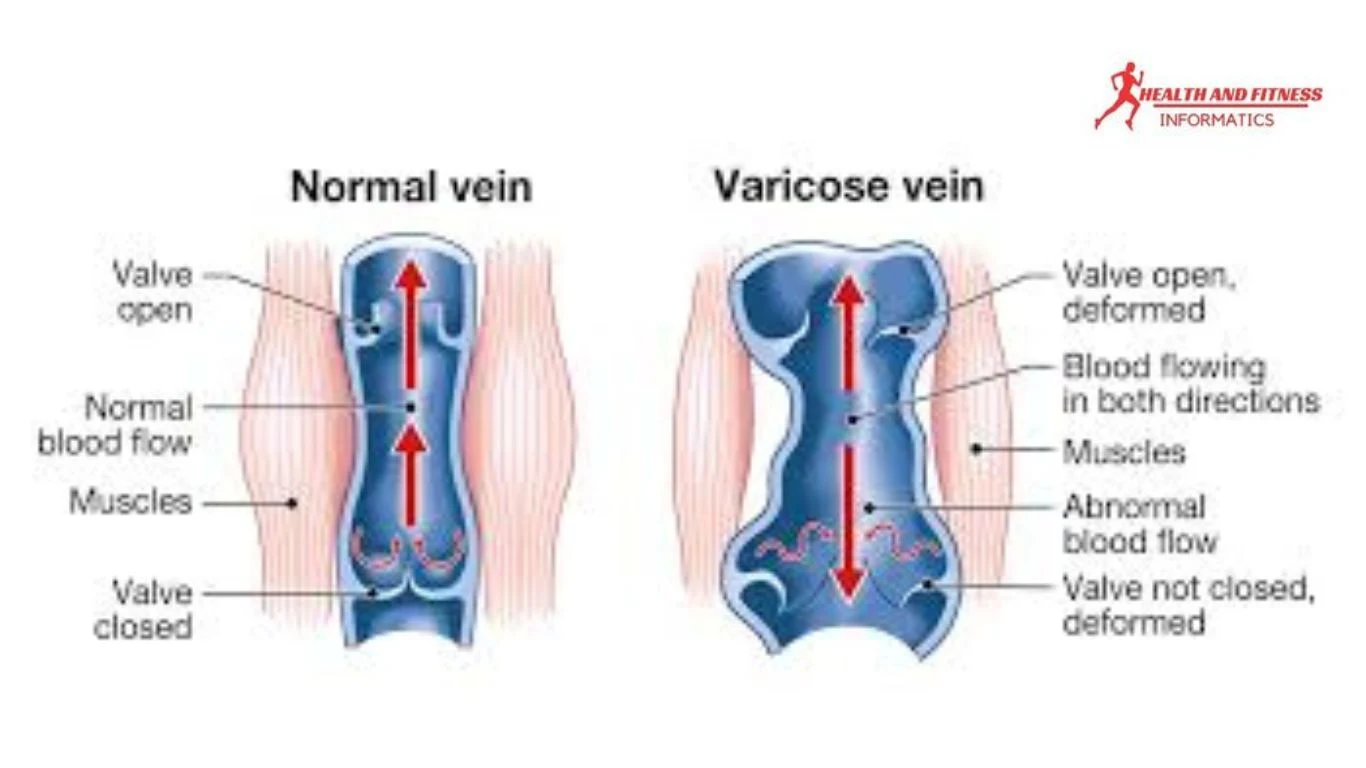
- Varicose veins in the legs or the genital region
- Swollen vulva
- Pelvic pain that worsens after certain physical activities, during menstruation, or after sex
- Pelvic pain gets worse as the day goes on, especially if you spend a lot of time standing
- Feeling a sudden need to urinate
Whwn your healthcare provier examine you, they may find your ovaries get tender and have abnormally swollen
veins in the vulva, back of the thigh, perineum, and buttocks1.
Causes:
What are the causes of PCS?
Healthcare experts are trying to figure
out what causes pelvic congestion syndrome.
- It seems that enlarged veins in the pelvis are a big part of it. However, many women have enlarged veins but don't have any symptoms.
- Pregnancy may elevate the chances of getting pelvic congestion syndrome because veins get bigger during pregnancy to handle more blood flow. This can make the veins permanently larger and lead to symptoms.
- Hormones may also have a role in pelvic congestion syndrome. For example, estrogen makes veins enlarger, which could explain why the condition is less common after menopause when estrogen levels are lower.
- Other hormones might also make veins wider and cause symptoms.
Diagnosis:
How is Pelvic congestion syndrome diagnosed?
Diagnosing pelvic congestion syndrome is
difficult as pelvic pain has many potential causes, including reproductive,
urinary, and gastrointestinal issues, muscles, bones, and mental health
conditions. Your healthcare provider will need to explore various possible
causes before making a diagnosis.
Your healthcare provider can diagnose the condition by taking your medical history and examining your symptoms. A pelvic exam is also likely to be conducted.
You may also need some tests, such as:
- Urine tests to check the urinary system
- Blood tests to check for sexually transmitted infections (STIs), pregnancy, anemia, and other conditions
- Pelvic ultrasound to look for growths in the pelvis
- Doppler ultrasound to check the blood flow in the pelvic blood vessels
- CT scan or MRI for more detailed pictures
- Diagnostic laparoscopy to rule out other causes of pelvic pain
- Magnetic resonance imaging/MR venography (MRI/MRV)
- Embolotherapy
Why Pelvic congestion syndrome is difficult to diagnose?
The diagnosis of pelvic congestion syndrome (PCS) poses a challenge for many doctors across various medical specialties, including anesthesia, gastroenterology, general surgery, obstetrics and gynecology, and interventional radiology. When other potential pelvic issues are ruled out, doctors may seek the expertise of an interventional radiologist for further evaluation and treatment of PCS. It's important for healthcare professionals to be more aware and suspicious of the specific symptoms and associated findings, as this can lead to a quicker progression toward treatment3.Editor's pick
What is Cicumvallate placenta?
Treatment:
How is pelvic congestion syndrome treated?
Your healthcare provider will determine the possible treatment options based on your symptoms. These options may include:- Progestin hormone therapy for pain relief
- Gonadotrophin-releasing hormone therapy to restrict ovarian function and pain relief
- Surgery to remove the ovaries and uterus
- Sclerotherapy and embolization, are procedures to remove/block veins.
At first, your healthcare
provider may prescribe medication. If that doesn't provide pain relief, they
may recommend a procedure to alleviate your symptoms as you enter menopause.
Although different doctors have different ways of performing this treatment, the main goal is to correct the veins in the ovaries, sometimes by making them shrink. Most of the treated women have experienced a 70 to 90% reduction in their symptoms, even though the treatment may vary slightly for each person2.
When should I call my healthcare provider?
If you suspect pelvic pain syndrome,
it's important to contact your healthcare provider if you experience any of the
following:
- Severe or sudden pelvic pain
- Pain that lasts for an extended period
- Pain that interferes with your daily activities
- Pain accompanied by fever, chills, or vomiting
- Pain that worsens or does not improve with home care or over-the-counter pain medication
It's essential to seek medical attention to receive an accurate diagnosis and appropriate treatment for pelvic pain syndrome.
What should I consider before visiting a healthcare provider?
Following key points you should keep in
mind before visiting your doctor such as:
- Understand why you're going and what you hope to achieve.
- Jot down any questions you have before your visit.
- Consider bringing a companion to help you remember important information.
- During your visit, take note of any new diagnoses, medications, treatments, or tests, as well as any instructions from your provider.
- Understand the purpose of any new medication or treatment, as well as its potential side effects.
- Inquire about alternative treatment options for your condition.
- Ask about the reasons behind recommended tests or procedures and what the results could indicate.
- Understand the potential consequences of not following through with prescribed medication, tests, or procedures.
- If you have a follow-up appointment, make sure to note the date, time, and purpose.
- Familiarize yourself with how to reach your healthcare provider in case you have any questions.
Conclusion:
Pelvic congestion syndrome is a
medical condition that leads to long-lasting pelvic pain. This condition is
believed to be caused by issues with the swollen veins in your pelvic region.
- Women of childbearing age who have had multiple pregnancies may be at the highest risk of developing pelvic congestion syndrome.
- The main symptom is pelvic pain, which may get worse after standing, walking, or having sexual intercourse. It could also begin during or after pregnancy.
- You might need to undergo several tests to eliminate other potential causes of pelvic pain.
- Symptoms may be alleviated with hormone treatments.
- Procedures such as blocking the damaged veins (embolization) or surgical removal of the ovary and tube or the uterus could be considered as options.





Post a Comment